Hip joint coxarthrosis (HJ) is a degenerative dystrophic disease that affects cartilage and bone tissue. In medical articles, it can be called differently: deforming coxarthrosis, hip joint AOD, osteoarthrosis. All of these terms mean the same pathology - arthrosis, but "coxarthrosis" is a more restricted concept that characterizes hip joint failure.
Cartilage is the first to suffer arthrosis, then bones and neighboring structures - ligaments and muscles - are involved in the pathological process. If there are changes in the bones, the prefix "osteo" is added to the word "arthrosis". In advanced cases, the joint is deformed, and there is already talk of deforming arthrosis (osteoarthrosis).
general features
Hip joint deforming osteoarthritis is the second most common after knee gonarthrosis. Due to the deep location of the hip joint, the bony deformity can go unnoticed for a long time, and only X-ray images taken in the later stages will show changes.
The development of this disease is influenced by several factors, including an inactive lifestyle, trauma and metabolic disturbances. It is because of the specifics of modern life, in which there is often no space for physical education, that arthrosis affects an increasing number of people. Furthermore, the peak of incidence falls in the middle-aged range - from 40 to 60 years.
Reference:coxarthrosis generally affects women than men.
development mechanism
The thigh joint is formed by two bones: the femur and the iliac (pelvic). The head of the femur enters the acetabulum of the pelvis, which remains immobile during movement - walking, running. At the same time, the articular surface of the femur can move in several directions, providing flexion, extension, abduction, adduction and rotation (rotation) of the thigh.
During physical activity, the femur bone moves freely in the acetabulum due to the cartilaginous tissue covering the joint surfaces. Hyaline cartilage is distinguished by its strength, firmness and elasticity; acts as a shock absorber and participates in load distribution during human movements.
Within the joint is the synovial fluid - the synovium - which is essential for lubricating and nourishing the cartilage. The entire joint is surrounded by a thin, dense capsule, surrounded by powerful muscles in the thighs and buttocks. These muscles, also acting as shock absorbers, serve to prevent injuries to the hip joint.
The development of coxarthrosis begins with changes in the joint fluid, which becomes more viscous and thicker. Due to the lack of moisture, the cartilage does not receive enough nutrition and starts to dry out, lose its smoothness and cracks appear.
Bones can no longer move as freely as they used to and rub against each other, causing microdamage to the cartilage. The pressure between the bones increases, the cartilage layer becomes thinner. Under the influence of increased pressure, bones are gradually deformed and local metabolic processes are disrupted. In later stages, there is pronounced atrophy of the leg muscles.
causes
Deforming arthrosis of the hip joint can be primary and secondary. It is not always possible to establish the cause of primary arthrosis. Secondary arthrosis appears in the context of existing diseases, namely:
- congenital hip dislocation or hip dysplasia;
- Perthes disease (aseptic necrosis of the femoral head);
- thigh arthritis of the hip joint, of infectious, rheumatic or other origin;
- pelvic bone injuries - dislocations, fractures.
Hip joint dysplasia is a congenital malformation that sometimes does not present clinically for a long time and in the future (at the age of 25–55 years) it can lead to the development of dysplastic coxarthrosis.
Lame arthrosis can be on the left, on the right and symmetrical. In primary arthrosis, concomitant diseases of the musculoskeletal system are frequently observed - in particular, osteochondrosis and gonarthrosis.
There are also risk factors that contribute to the onset of the disease:
- overweight and excessive loads that strain the joints;
- disturbance of blood circulation and metabolism;
- hormonal changes;
- spinal curvature, flat feet;
- advanced age;
- hypodynamics;
- heredity.
It should be noted that coxarthrosis itself is not hereditary. However, certain characteristics of metabolism or connective tissue structure may create prerequisites for the development of arthrosis in a child in the future.
Symptoms of coxarthrosis
The main symptom of arthrosis of the hip joint is pain in the hip and groin region, which varies in intensity. Stiffness and stiffness during movement, decreased muscle volume, shortening of the affected limb and gait alteration due to lameness are also observed.
The coxarthrosis usually progresses slowly, causing discomfort at first and mild pain after exertion. However, over time, the pain increases and appears at rest.
A typical manifestation of pathology is difficulty with hip abduction, when the person cannot sit "straddled" in a chair. The presence and severity of the signs of coxarthrosis depend on its degree, but the painful syndrome is always present.
There are three degrees or types of arthrosis of the hip joint, differing in the severity of the injury and accompanying symptoms:
- 1 degree. The thigh doesn't hurt all the time, but periodically, especially after walking or standing for a long time. The pain syndrome is located in the area of the joint, but it can sometimes spread up the leg to the knee. Muscles with 1st degree coxarthrosis do not decrease in size, gait does not change, motor skill is completely retained;
- 2nd degree. The sensations of pain intensify, appearing not only after running or walking, but also at rest. The pain is most often concentrated in the thigh region, but may spread to the knee. In moments of great load, it is painful to step on the injured limb, so the patient begins to spare his leg and limps. The range of motion in the joint decreases, it is especially difficult to move the leg to the side or rotate the hip;
- 3 degrees. The pain becomes permanent and doesn't even subside at night. Gait is visibly impaired, independent movement is significantly complicated, and the patient leans on a cane. Range of motion is severely limited, muscles in the buttocks and the entire leg, including the leg, atrophy.
- Due to muscle weakness, the pelvis tilts forward and the affected leg is shortened. To compensate for the difference in limb length, the patient bends the body to the affected side when walking. This leads to a shift in the center of gravity and increases stress on the affected joint.
Osteoarthritis or Osteoarthritis?
Arthritis is inflammation of the joint, which can be an independent disease or develop in the context of systemic pathologies (eg, rheumatism). In addition to the inflammatory response, symptoms of osteoarthritis (especially in the advanced stages) include limited mobility and changes in the shape of the joint.
At the heart of the degenerative dystrophic changes in arthrosis is the defeat of cartilage tissue, which often leads to inflammation. This is why osteoarthritis is sometimes called arthrosis-arthritis. And as arthrosis is almost always associated with joint deformity, the term "osteoarthrosis" is applicable to it.
Reference:according to the International Classification of Diseases (ICD-10), osteoarthritis and osteoarthritis are varieties of the same pathology.
Diagnosis of coxarthrosis
The diagnosis of "coxarthrosis of the hip joint" is made based on the test, the patient's complaints, and the test results. The most informative method is the X-ray: in the photos you can see the degree of damage to the joint and the cause of the disease.
For example, in hip dysplasia, the acetabulum is flatter and more inclined, and the cervico-diaphyseal angle (inclination of the femoral neck in the vertical plane) is greater than normal. Deformity of the part of the femur located in the vicinity of the joint is characteristic of Perthes disease.
3rd degree coxarthrosis is characterized by a narrowing of the joint space, expansion of the femoral head and multiple bone growths (osteophytes).
If the patient has had a fracture or dislocation, signs of trauma will also be visible on radiographs. If a detailed assessment of bone and soft tissue condition is required, MRI or CT scan may be prescribed.
Differential diagnosis is performed with the following diseases:
- gonarthrosis;
- osteochondrosis and radicular syndrome arising in its background;
- trochanteritis (inflammation of the trochanter bone of the thigh);
- ankylosing spondylitis;
- reactive arthritis.
The decrease in muscle volume that accompanies the 2nd and 3rd degrees of coxarthrosis can cause pain in the knee region. In addition, the knee tends to hurt even more than the hip joint itself. To confirm the diagnosis and exclude gonarthrosis, an x-ray is usually sufficient.
With spinal disorders - osteochondrosis and pinched nerve roots - the pain is very similar to coxarthrosis. However, it occurs unexpectedly, after an unsuccessful movement, an abrupt turn of the body or weight lifting. Pain sensations start in the gluteal region and spread to the back of the leg.
Root syndrome is characterized by severe pain when lifting a straight limb from the supine position. However, there are no difficulties during leg abduction to the side, as in coxarthrosis. It is important to note that osteochondrosis and arthrosis of the hip joint are often diagnosed simultaneously, so a comprehensive examination is needed.
Trochanteritis, or trochanteric bursitis, develops rapidly, unlike arthrosis, which can progress slowly over years and even decades. The pain syndrome increases in a week or two, although it is quite severe. The cause of trochanteritis is trauma or excessive exercise. Movement is not limited and the leg is not shortened.
Ankylosing spondylitis and reactive arthritis may also be accompanied by symptoms that mimic coxarthrosis. The hallmark of such illnesses is the appearance of pain, especially at night. The hip can hurt a lot, but as you walk and move, the pain lessens. In the morning, patients are concerned about stiffness, which disappears after a few hours.
Treatment of arthrosis of the hip joint
The coxarthrosis can be cured conservatively or surgically. The choice of treatment method depends on the stage and nature of the course of the pathological process. If diagnosed with 1 or 2 degrees of the disease, it is treated with medication and physical therapy. After the relief of acute symptoms, therapeutic exercises and massage are added. If necessary, a special diet is prescribed.
The earlier coxarthrosis is detected and treated, the more favorable the prognosis. With the help of medications and therapeutic measures, you can significantly delay the pathological process and improve your quality of life.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are used to relieve pain and inflammation. It is noteworthy that anesthesia is performed in the shortest time possible, since drugs of the NSAID class can negatively affect the digestive tract and delay the processes of cartilage tissue regeneration.
It is possible to speed up the restoration of cartilage with the help of chondroprotectors. However, these funds are only effective in the early stages of the disease, when your hyaline cartilage is not completely destroyed. Chondroprotective drugs are prescribed in the form of pills or intra-articular injections.
To improve the blood supply to the joint, vasodilators are used. For muscle spasms, muscle relaxants are recommended.
For persistent pain syndrome, which is difficult to eliminate with pills, injections are made into the hip joint. Corticosteroids also relieve inflammation and pain.
Drug therapy can also be complemented with topical agents - ointments and gels. They do not have a pronounced effect, but they help to deal with muscle spasms and reduce pain.
Physical therapy helps improve blood circulation and cartilage nutrition. For coxarthrosis, procedures such as shock wave therapy (SWT), magnetotherapy, infrared laser, ultrasound, and hydrogen sulfide baths have been shown to be excellent.
Operation
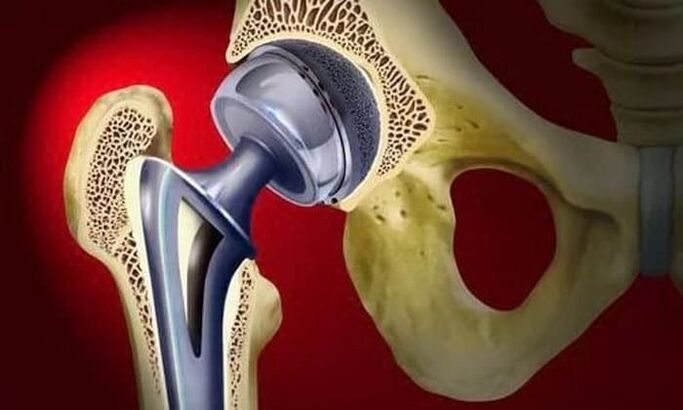
The treatment of stage 3 osteoarthritis can only be surgical, as the joint is almost completely destroyed. To restore function to the hip joint, partial or total arthroplasty is performed.
Surgical treatment is used in advanced cases of arthrosis, when conservative therapy is impotent.
In partial prostheses, only the head of the femur is replaced by an artificial prosthesis. Total prosthesis means replacing the femoral head and acetabulum. The operation is performed under general anesthesia and, in the overwhelming majority of cases (about 95%), hip joint function is fully restored.
During the rehabilitation period, the patient is prescribed antibiotics to prevent infectious complications. The stitches are removed on day 10-12 and exercise therapy is started. The attending physician helps the patient to learn to walk and correctly distribute the load on the operated limb. Exercise is an important step in increasing muscle strength, endurance and elasticity.
Working capacity is restored on average 2-3 months after the operation, but for older people this period can be up to six months. After rehabilitation is complete, patients can move, work, and even play sports. The useful life of the prosthesis is at least 15 years. To replace a worn prosthesis, a second surgery is performed.
Effects
Without timely and adequate treatment, coxarthrosis can not only significantly worsen quality of life, but also lead to disability and incapacity. In the second stage of arthrosis, the patient moves to the 3rd group of disability.
When shortening the affected limb by 7 cm or more, when a person moves only with the help of improvised means, a second group is assigned. The 1st group of disabilities is taken in by patients with 3rd degree coxarthrosis, accompanied by complete loss of motor capacity.
Indications for medical and social examination (MSK) are:
- long course of arthrosis, more than three years, with regular exacerbations. The frequency of exacerbations is at least three times every 12 months;
- submitted to endoprosthesis surgery;
- severe disorders of the musculoskeletal function of the limb.
Prophylaxis
The main measures to prevent coxarthrosis are diet (if you are overweight) and regular but moderate physical activity. It is very important to avoid injuries to the pelvic region and hypothermia.
In the presence of risk factors for the development of arthrosis, as in all patients with diagnosed disease, swimming is beneficial. Sports such as running, jumping, soccer and tennis are not recommended.

























