Unnatural changes in the cartilage and bones of the spine cause the development of the disease, which, according to the ICD-10 code, refers to the location of M42 and is called thoracic osteochondrosis. The middle part of the spine is less stressed than the lumbar and cervical spine, but deformities are difficult to cure. The load is unevenly distributed due to the rounded configuration of the sternum, osteophytes and other dysplastic manifestations appear.
Symptoms and Signs
The disease occurs in the nucleus pulposus of the intervertebral disc, spreads to the fibrous fibrous ring and other parts of the vertebral segment, which ensure spinal mobility. Changes are manifested by compression, reflex or mixed neurological disorders, and syndromes.
Pain manifests with physical exertion. There are different types of sensations:
- prolonged mild pain in the chest region is called back pain;
- acute and sharp colic, causing a difficult inhalation or exhalation, leading to immobility of muscles - back.
The symptoms and treatment of osteochondrosis of the thoracic spine depend on the degree of wear of the bone apparatus and the stage of aging, which are generalized and local.
Symptoms include:
- damage to peripheral nerve processes (neuralgia), characterized by painful attacks along the intercostal vasoconstrictors;
- concentration of pain on the left side of the chest or occurrence of severe herpes zoster-like painful sensation;
- decreased mobility of the spine in the chest region;
- numbness in arms and hands;
- decreased sexual function;
- the appearance of pain in the area of Organs internal organs, it can give to the heart, stomach, liver;
- lumbago in the neck, cheekbones and head, cough or a lump in the throat;
- arrhythmia, tachycardia, fever.
The signs of osteochondrosis are disguised as manifestations of related illnesses, so the symptoms are ambiguous. Spinal nerves are concentrated around the spine; when pinched, signals are sent to different parts of the body and organs.
Causes of osteochondrosis
There is no exact information on which factors deform the intervertebral discs. A common reason for osteochondrosis is scoliosis or curvature of the spine, which is most often seen in childhood and adolescence.
The theory considers these vertebral deformity factors:
- dysontogenetic;
- hormonal;
- vascular;
- functional;
- involutive;
- infectious;
- immune;
- dysmetabolic;
- mechanical;
- hereditary.
Deterioration and aging of bones and cartilage occur as a result of prior exposure to adverse conditions. Atrophic spinal degenerations are predetermined by a genetic factor, and a disease with clinical symptoms arises under the influence of an exogenous and endogenous environment.
The consequence in the form of complications in the work of the vertebrae occurs when the process of destruction of complex substances prevails over their synthesis. An exacerbation occurs when the disk's power supply is interrupted and there is a shortage of useful elements. Penetration of elements and dissimilation products decreases, cell viability decreases and parts of cells accumulate due to self-destruction. The production of complex proteins is reduced, collagen fibers are destroyed.
The mechanical effect on the formation of the annular connective increases, the layered structure is disorganized, the fibrous skeleton is torn. The disc is bruised under the influence of biomechanical factors and body movements, and its fixation capacity is diminished. Blood vessels and nerves can grow into the ring due to a decrease in hydrostatic pressure.
diagnostic methods
In the recognition process, root, painful, reflex, myotonic, autonomic and vascular factors are identified. The best method of examination is difficult to identify, as the diagnosis is made individually in each case.
The main methods are:
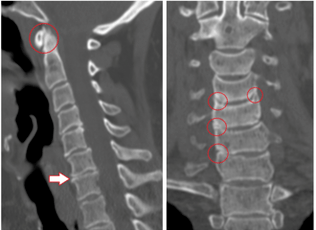
- X-ray diagnosis;
- Computed tomography;
- Magnetic resonance imaging.
The X-ray analyzes the condition of the spine, images are provided in oblique, lateral and direct projections. Sometimes, for a photo, a person bends, unfolds, or leans to the side.
Contrast radiography is divided into the following studies:
- pneumomyelography - 20 to 40 ml of air is injected into the spinal canal;
- angiography - 10 ml of contrast agent is injected into the spinal lumen and 7 to 9 images are taken in 2 to 3 seconds;
- myelography - an injection of a dye fluid is made into the subarachnoid lumen, followed by a transillumination of the structure;
- discography - the stained substance is injected directly into the disc for localized examination.
Computed tomography assesses bone and tissue structure, the state of blood vessels. The painless method obtains three-dimensional images in a few minutes.
CT Benefits:
- high detection speed;
- screening for "dumb" areas during ongoing diagnoses;
- the possibility of multispiral angiography;
- recognition of long objects by obtaining high quality thin slices.
Magnetic resonance imaging uses the magnetic field of a machine that builds hydrogen atoms in the human body in parallel with the action. The particles signal, the response is registered. The CT scanner recognizes the waves and shows the result on the screen. With MRI, there is no radiation, the method is less dangerous, but it is not recommended for pregnant women.
treatment and prevention
It is necessary to treat osteochondrosis in several stages, the complexity depends on the severity of the disease, contraindications and body resources.
Methods:
- drugs and medications;
- physiotherapy methods, clamp removal exercises, relieving the patient's condition;
- Operation.
There is a direction of kinesiotherapy, within which it is possible to cure spinal problems in the form of a hernia, spondylosis with rehabilitation gymnastics. In addition, a method of recovery after surgery has been developed.
Yoga exercises help men, women and children to overcome pain, warning that the main thing is a psychological attitude.
Medicines
Medications are prescribed by the neurosurgeon or neuropathologist according to the chart and medical history. Patients take their medications in the hospital or at home, the main thing is to follow the instructions and not deviate from the intake regimen.
Common medications:
- NSAIDs relieve pain, fever and inflammation;
- muscle relaxants reduce skeletal muscle tone;
- hormones reduce neuralgic pain;
- vitamins B2, B6, B12, A and C are taken during remission and for simple prophylaxis;
- diuretics relieve swelling and release pinched root nerves;
- neurometabolic stimulants improve metabolism in nervous tissues;
- chondroprotectors restore cartilage to the vertebrae after damage.
Sometimes the patient goes without medication in the first phase of the onset of unpleasant sensations. Just exercise, use a massager.
Physiotherapy

This type of exposure is used in conjunction with drug treatment or separately. Also, bed rest is applied, heat is applied to the affected area. Popular recipes are used to relieve pain.
Physical therapy in a medical institution includes procedures:
- ultrasound and phonophoresis;
- shock wave therapy;
- impact of the detainer;
- laser therapy;
- electrotherapy;
- magnetic waves;
- mud therapy and balneotherapy;
- massage.
Ultrasound involves the effect of high frequency waves on tissues, which reduces pain sensitivity. With ultraphonophoresis, analgesics and anti-inflammatory drugs are added for better distribution in the affected areas.
Shockwave therapy is the transmission of an acoustic wave to the painful area, it is used to improve blood circulation, speed up metabolism. Detensor therapy consists of lengthening the spine using the patient's body weight.

Laser therapy is based on the generation of a helium-neon laser to activate bioelectric currents in nerve fibers. The laser acts on the inflamed nerve roots in the paravertebral region along the thoracic region.
Electrotherapy improves nutrition and product metabolism in tissues, and impulse currents affect sensory nerve endings. Low frequency waves relieve acute pain and are used as an initial aid.
Magnetic therapy is used to relieve swelling, spasms, and inflammation. A magnetic wave inducer is placed in the affected chest region. Balneotherapy and fangotherapy consist of swimming in pools, bathing, contrast showers for treatment and during recovery. Metabolism is normalized, blood flow to the affected areas is accelerated, pain and inflammation are reduced.
Therapeutic massage for osteochondrosis of the thoracic spine is vacuum, punctual and lymphatic drainage, improves blood microcirculation, tissue nutrition and tones muscles. Sessions are conducted by a competent expert; if you entrust the backbone to amateurs, dangerous consequences can occur. Massage is prescribed after the end of the acute phase, the first session should not exceed 10 minutes.
surgical treatment
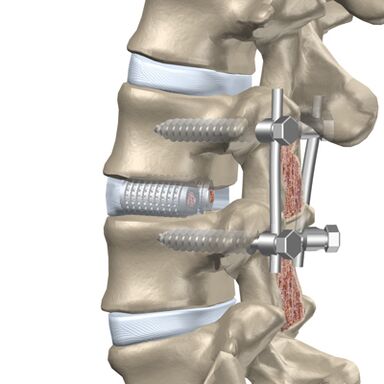
The patient is referred for an operation if medical treatment, massage, and other procedures do not alleviate the condition.
The intervention is divided into 2 steps:
- elimination of the cause of intense pain (decompensation);
- spinal stabilization.
Through the posterior route, a facetomy is performed, as the joints can put pressure on the nerves. Foraminotomy is the expansion of the root canal through which the nerve leaves the vertebra. Laminectomy removes the posterior portion of the vertebra, which protects the spinal lumen and puts pressure on the brain due to the deformity. Laminotomy involves widening the opening of the canal, where the spinal cord is located, while removing a separate fragment from the posterior region of the vertebra.
Anterior surgery is performed if there is a protrusion (protrusion of the vertebral disc into the spinal lumen) or a hernia protrudes into the canal.
The following methods are used for frontal decompression:
- discectomy - removal of an entire disc or a separate part of it;
- corpectomy - removal of an entire vertebra and adjacent disc followed by implantation.
Discectomy and corpectomy lead to spinal destabilization and increase the risk of neurological defects. Rigid fixation or fusion of three vertebrae (fusion) is used.
Prevention of Thoracic Osteochondrosis

Disease exacerbations reduce human work capacity and quality of life, therefore, special attention is paid to prevention. As a result, vertebral degeneration appears later and deficiency is avoided.
Methods to prevent the disease:
- decreased physical activity in the spine;
- you can't stand still for long without changing the support member, you can lean on a makeshift object or a wall;
- it is not recommended to sit at the table for a long time and, when working with the computer, it is necessary to take active breaks, take a walk;
- orthopedic mattresses and headrests are selected for sleeping;
- when running and walking, you need to avoid sudden turns and jumps, walk in shock absorbing shoes and with small heels;
- carry weights not exceeding 10 kg, gradually rise from a sitting position.
In the car, it is necessary to use backrests and headrests, while the driver's seat must be rigid. The work cannot be done in a half incline position, you can stand or sit. Well-developed muscles support the skeleton, so they pay attention to viable physical education and hardening.
possible complications
The disease develops for a long time, sometimes the pain symptoms do not appear immediately. Any degenerative changes in the thoracic region lead to the appearance of pathologies.
Types of complications:
- pathology of cardiac vessels with subsequent myocardial infarction or angina pectoris;
- intercostal neuralgia or inflammation of the peripheral nerves with chest pain from root compression;
- protrusion of intervertebral discs.
Complications occur with advanced forms of osteochondrosis, so timely treatment in the early stages will help to prevent concomitant illnesses.

























